Spinal injections are important for evaluating and managing spinal pain. Precision image–guided injections can be helpful and at times are essential to help localize the structural origin of a patient’s pain. If a pain source or pain generator is identified, injections can be useful therapeutic adjuncts in properly selected patients.
Identification and localization of the source of pain in patients presenting with spinal pain can be a vexing diagnostic challenge. Often, it is not possible to localize the source of a patient’s pain by routine clinical evaluation. For example, patients with painful sacroiliac arthropathy may present with symptoms identical to those of patients who have either diskogenic pain or pain originating in the zygapophyseal joint (also called the facet joint or z joint). Several studies have confirmed that it is impossible to accurately differentiate lumbar z joint pain, sacroiliac pain, and diskogenic pain solely by history and physical examination. The fact that radiographic findings are often nonspecific further complicates diagnostic evaluation.
Diagnostic injections can help determine whether a pathologic structure or so-called pain generator is contributing to a patient’s pain. Lack of temporary pain relief after a properly performed diagnostic local anesthetic block is evidence that a structure other than the one injected is the pain generator. Conversely, pain relief after a properly controlled diagnostic injection is important evidence that the anesthetized structure is a pain generator for that patient. Several studies have shown that response to anesthetic block of the sacroiliac and z joints is the best diagnostic test for determining the contribution of these structures to a patient’s pain. Similarly, selective spinal nerve blocks can be used to help identify the source of radicular pain when clinical examination and radiographic studies are not diagnostic.
masculinely Zygapophyseal Joint Injections and Blocks
Epidemiological studies have implicated the z joint as a source of pain in 15% to 40% of patients presenting with low back pain. The most common causes of z joint pain are osteoarthritis, sprain (capsule or ligament injury), and inflammatory synovitis. To determine whether z joints are contributing to a patient’s pain, intra-articular anesthetic block or local block of the medial branch nerves that innervate the z joints can be used. In most cases, medial branch nerve block is the preferred diagnostic block and has proven diagnostic validity and specificity. If there is no change in pain after a diagnostic block, the injected joint is unlikely to be the source of pain, and attention can be directed elsewhere. If pain is relieved, the injected joint may be contributing to the patient’s pain.
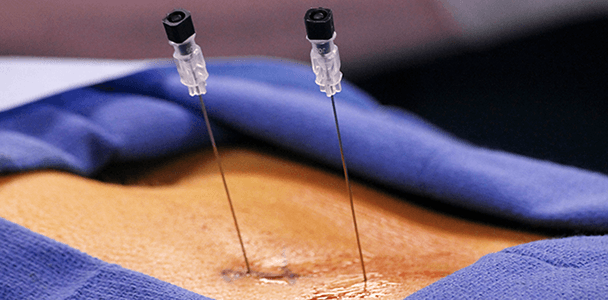
Therapeutic exercise, activity modification, and medical therapy constitute initial conservative treatment of z joint pain. Joint injections and nerve blocks are useful in patients who do not respond to conservative therapy. Intraarticular local anesthetic and corticosteroid injections can be helpful in patients with MRI-confirmed z joint synovitis. Radiofrequency neurotomy of the medial branch nerve is effective in the treatment of intractable z joint pain. This minimally invasive procedure involves fluoroscopically guided placement of a specially designed needle electrode next to the medial branch nerves of the offending z joint or joints. A high-frequency (500 kHz) current is generated at the tip of the electrode, which heats and thermally damages the medial branch nerve. A recent study of more than 600 radiofrequency treatments revealed no major complications from this technique. The major limitation is neural regrowth, with a possible return of symptoms.
Tangkak Epidural and Spinal Nerve Injections and Blocks
Selective spinal nerve blocks can be helpful in diagnosing lumbar radiculopathy,46 particularly when the nerve rot or roots contributing to the pain cannot be determined convincingly by history, examination, electrodiagnostics, or radiographic studies. Many patients with lumbar radiculopathic symptoms present with complex radiographic findings and equivocal or nondiagnostic electromyographic findings. A typical example is a patient who has radicular pain with multilevel foraminal narrowing and multilevel degenerative disk disease, such that the pain-generating level is indeterminate. A carefully performed fluoroscopically guided or CT-guided selective nerve block with local anesthetic can help to localize the involved nerve root. Failure to obtain relief after a block is evidence that the pain is originating elsewhere. If pain is relieved after the block, the injected nerve may be contributing to the patient’s pain. A caveat to consider when interpreting the outcome of a diagnostic block is that it is possible for the injected anesthetic to spread to adjacent spinal levels.
Selective spinal nerve injections and epidural injections also may be used therapeutically. The most common therapeutic indication is treatment of painful lumbar radiculopathy that has not responded to more conservative spinal care measures. Most patients with lumbar radiculopathy improve without surgery. However, many of these patients have pain that is difficult to control with medications and physical therapy. Such patients can benefit considerably from injection therapy. Although the pain mechanisms in lumbar radiculopathy may be complex and multifactorial, a large body of evidence shows that nerve root inflammation plays an important role. Accordingly, the application of perineural corticosteroids can reduce inflammation and improve pain symptoms. When combined with activity modification and an appropriate rehabilitation program, epidural injections can reduce pain, hasten recovery, and reduce the likelihood of surgery. However, patients with severe or progressive neurologic deficits related to nerve compression should be considered candidates for surgery rather than for injection therapy.
the 2 most common injection approaches are interlaminar epidural corticosteroid injection and transforaminal epidural corticosteroid injection. (The transforaminal epidural corticosteroid injection technique is similar to selective spinal nerve block.) Each technique has its advantages and disadvantages, but the goal of both is to deliver the therapeutic solution (in most cases, a corticosteroid) to the putative inflamed nerve. Both techniques require fluoroscopic guidance to ensure that the solution reaches the intended target. No comparative studies show superiority of one technique over the other. Patient circumstances may influence the choice of approach. For example, a transforaminal approach may be preferred in patients who have previously undergone spinal surgery near the area to be injected, whereas an interlaminar approach may be preferred in patients with severe foraminal narrowing that may limit the spread of the therapeutic solution to the desired location. In some cases, a radiopaque catheter is guided through the epidural space to the targeted nerve, and the therapeutic solution is delivered through the catheter. Patients who do not improve after conservative spinal care measures and injection therapy may be candidates for surgery.
أضف تعليقك